Beyond Subsidies: How the GOP’s HSA Plan Could Quietly Reshape American Health Care

Sarah Johnson
December 9, 2025
Brief
A deep analysis of Senate Republicans’ push to replace Obamacare subsidies with HSAs, unpacking who wins, who loses, and how culture-war riders could reshape U.S. health policy.
Why Republicans Want to Swap Obamacare Subsidies for Health Savings Accounts—and What That Really Means
At first glance, Senate Republicans’ new proposal to replace expiring Affordable Care Act (ACA) premium subsidies with pre-funded Health Savings Accounts (HSAs) looks like just another skirmish in the long-running Obamacare wars. In reality, it’s something more consequential: an effort to structurally reshape how federal help for health coverage is delivered, who benefits, and which culture-war priorities are baked into the health-care financing system itself.
Understanding this fight requires seeing past the rhetoric—“give money to patients, not insurance companies”—and examining how HSAs actually work, who uses them, and how the proposal links technical insurance policy to hot-button issues like immigration, abortion, and gender-affirming care.
The bigger picture: A decade-long battle over how (and whether) to subsidize health care
The Cassidy–Crapo plan is the latest iteration of a 15-year ideological divide over the federal government’s role in health insurance. Since the ACA passed in 2010, the central questions have been:
- Should federal support flow primarily through regulated insurance markets (subsidies, Medicaid expansion, essential health benefits), or through tax-advantaged accounts and private choice mechanisms?
- Should aid be more generous and targeted to lower- and middle-income people, or more evenly spread and conditioned on individual responsibility (like opting into high-deductible plans)?
The Biden-era ACA subsidy enhancements—originally enacted as part of COVID relief—answered those questions in one direction: bigger, broader subsidies that made ACA plans cheaper, especially for middle-income families. The result was a record 21+ million people enrolled in marketplace plans and historically low uninsured rates near 7.2% in 2023, according to federal data.
Those subsidy boosts are now expiring. Democrats want to extend them; Republicans want to redirect that same money into HSAs seeded with $1,000–$1,500 per person for those buying bronze or catastrophic exchange plans.
Viewed in historical context, this is less a technocratic tweak than a philosophical reversal: from subsidizing comprehensive coverage upfront to subsidizing out-of-pocket spending in a more consumer-directed framework.
How the Cassidy–Crapo plan would change the playing field
The core mechanics of the proposal are straightforward on paper:
- Replace ACA premium subsidies (enhanced under Biden) with federal contributions into HSAs.
- Deposit $1,000 per person ages 18–49, and $1,500 for ages 50–65, for people earning up to 700% of the federal poverty level (FPL) who buy a bronze or catastrophic plan on an ACA exchange.
- Layer in policy riders: cuts to Medicaid funding for states covering undocumented immigrants; stricter citizenship verification; bans on federal Medicaid funding for gender-transition services and exclusion of those services from essential health benefits; and Hyde-style abortion funding restrictions for the new HSAs.
The political pitch is simple: stop sending “billions” to insurers and give money directly to patients. But there are three under-discussed implications.
1. HSAs favor people with cash and higher incomes
HSAs are tax-advantaged accounts: contributions are pre-tax, growth is tax-free, and withdrawals for medical expenses are untaxed. That structure disproportionately benefits people with higher marginal tax rates and enough disposable income to contribute beyond any federal seed money.
Under this plan, lower-income enrollees would indeed get a $1,000 or $1,500 deposit. But if the enhanced ACA subsidies expire, many of those same people will face sharply higher premiums. Those higher premiums don’t come out of HSAs—they’re paid separately. The seed money primarily offsets deductibles and copays, not the monthly cost of staying insured.
In practical terms, a family that currently pays near-zero premiums thanks to subsidies could be forced to choose: pay substantially more each month for a bronze plan to unlock an HSA deposit, or drop coverage altogether. The federal deposit will not match the value of the lost premium subsidy for many low- and middle-income households.
2. The bronze/catastrophic requirement nudges people toward skimpier coverage
Conditioning the HSA deposit on enrollment in bronze or catastrophic plans is not a neutral design choice. Bronze plans often have deductibles in the $7,000–$9,000 range per person. A $1,000 deposit is helpful, but it barely makes a dent in those deductibles, especially for those with chronic illnesses.
Democrats have spent years trying to push consumers into silver and higher-tier plans to improve actuarial value—i.e., how much the plan actually pays when care is needed. The Cassidy–Crapo structure pulls in the opposite direction: more people in low-premium, high-deductible coverage, buffered only slightly by a one-time deposit.
That shift matters because high deductibles are already associated with people delaying or avoiding needed care. A 2022 Kaiser Family Foundation survey found that half of insured adults with high deductibles said they or a family member skipped or delayed care because of cost in the previous 12 months.
3. Culture-war riders convert a subsidy fight into a broader ideological test
The bill doesn’t just change the financial architecture of ACA support; it weaponizes it for broader policy goals:
- Immigration: Reducing federal Medicaid funds to states that cover undocumented immigrants raises the stakes for so-called “sanctuary” health policies and could chill state efforts to provide basic care to mixed-status families.
- Transgender care: Banning Medicaid funding for gender-transition-related services and removing them from essential health benefits effectively uses the ACA fight as a vehicle to narrow access to gender-affirming care, even for privately insured people.
- Abortion: Extending Hyde-style restrictions to the new HSAs embeds abortion politics into yet another federal health financing stream, complicating how individuals use their own accounts when federal dollars are involved.
By attaching these policies to an HSA-based replacement, Republicans aren’t just offering an alternative to subsidies; they’re trying to reset the moral contours of federally supported health care. That bundling makes bipartisan compromise far harder, even among senators who might be open to tweaking subsidies.
What Republicans are really trying to solve—and what they’re not
Republican sponsors argue that current subsidies have failed to control premiums and primarily enrich insurers. There is some truth to the concern: ACA premiums have risen, and federal subsidies do ultimately flow through enrollees to insurers.
But the proposal sidesteps three structural drivers of U.S. health costs:
- Provider prices: Hospitals and physician groups in consolidated markets can command higher prices. Neither HSAs nor subsidies directly address provider consolidation or price transparency in a meaningful way.
- Drug prices: Pharmaceutical spending continues to strain both public and private budgets. The proposal doesn’t materially confront pharmaceutical pricing or patent loopholes.
- Administrative overhead: Fragmented insurance arrangements and complex billing drive up administrative costs—an estimated 15–25% of total health spending. Again, the HSA shift leaves that untouched.
Instead, the plan focuses on perceived “moral hazard” on the consumer side: the belief that if people have more “skin in the game” via HSAs and high deductibles, they’ll shop more carefully and avoid unnecessary care. Evidence for this is mixed. Research on high-deductible plans shows that while people do cut back on care, they often reduce both low-value and high-value services, including preventive care they actually need.
The proposal also frames premium subsidies as inherently flawed because they’re paid through insurers. That ignores a basic feature of insurance markets: unless the federal government directly runs a public plan, subsidies will always flow through private or nonprofit carriers. The policy question isn’t whether insurers receive money; it’s whether subsidized coverage produces better health and financial protection than the alternatives.
Who wins, who loses: likely distributional effects
Without detailed Congressional Budget Office modeling, impacts can only be approximated, but some patterns are likely:
- Higher-income, healthier individuals who already favor high-deductible plans would likely benefit from extra HSA seeding, building on existing tax advantages.
- Lower- and moderate-income enrollees who currently rely on enhanced ACA subsidies to keep premiums low could face higher monthly costs. The HSA seed may not fully offset the loss of premium support, especially for older adults in high-cost areas.
- People with chronic conditions might find that the combination of bronze coverage and modest HSA deposits leads to greater out-of-pocket exposure and more financial risk.
- Insurers could see a shift in risk pools if healthier people gravitate toward HSA-tied bronze plans while sicker individuals struggle to maintain more comprehensive coverage.
In short, the proposal nudges the system toward greater individual exposure to costs, with relatively more gain for the healthy and higher-income, and more risk for those already on the financial edge.
Expert perspectives: ideology versus evidence
Health policy experts have long debated HSAs and high-deductible plans. The divide is less about whether HSAs can be useful—many analysts agree they can—and more about whether they should be the backbone of federal support for health coverage.
Economist Jonathan Gruber, who helped design the ACA, has noted in past analyses that “high-deductible, consumer-directed plans do reduce spending, but they do so by discouraging use across the board, not by making consumers better shoppers.” In other words, you get less care overall, not necessarily smarter care.
Conservative scholars at places like the American Enterprise Institute and the Heritage Foundation, by contrast, have argued that HSAs restore consumer autonomy and can limit unnecessary utilization. They tend to view ACA subsidies as entrenching a heavily regulated insurance regime that suppresses innovation and overprotects carriers.
The Cassidy–Crapo proposal is firmly in that conservative tradition. The question is whether the ideological faith in price-sensitive consumers matches the lived reality of people navigating surprise bills, opaque prices, and medical emergencies where shopping around simply isn’t possible.
Looking ahead: policy, politics, and the risk of coverage cliffs
In the near term, the key question is whether any of the competing Republican plans can coalesce into a single position—and whether Democrats will entertain any move away from extending current subsidies. The inclusion of immigration, abortion, and gender-care provisions makes a bipartisan deal less likely, at least in the short run.
Three broader risks are worth watching:
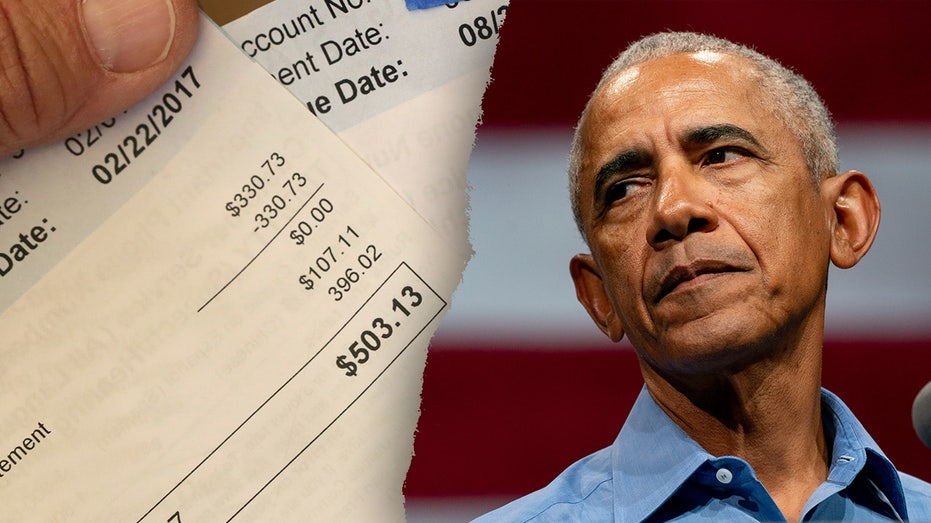
- The coverage cliff: If enhanced subsidies expire without a viable, adequately funded replacement, millions could see double-digit premium increases at their next renewal. That’s not abstract; a previous lapse in enhanced subsidies in 2017–2018 led to measurable coverage losses.
- Fragmentation of ACA rules across states: Tying Medicaid funding to immigration enforcement and banning certain types of care could further fragment the national health policy landscape, with residents’ access to services increasingly determined by state politics.
- Normalization of culture-war riders in core health financing bills: Once abortion and gender-affirming care are routinely inserted into foundational financing debates, it becomes harder to negotiate purely on economic or actuarial grounds. Health policy becomes a proxy for broader cultural conflict.
Even if this specific proposal stalls, it signals where Republican health policy is headed: away from premium-based subsidies toward consumer-directed accounts, and toward a model where access to coverage is more tightly linked to ideological conditions on what care can be covered and for whom.
The bottom line
The Senate Republican plan to swap Obamacare subsidies for HSAs is not just about how to spend a pot of federal money. It’s a bid to rewire the basic circuitry of U.S. health coverage: from pooled risk and upfront premium assistance to individualized accounts, higher deductibles, and an explicit layering of immigration, abortion, and gender-care restrictions into the core of the system.
Whether that vision prevails will determine not only how much Americans pay for care, but how much ideological litmus tests shape who gets help, and on what terms, when they get sick.
Topics
Editor's Comments
One underappreciated dimension of the Cassidy–Crapo proposal is how it redefines the political constituency for federal health aid. Premium subsidies create a broad coalition: they quietly support millions of lower- and middle-income households, many of whom may not even realize how much they benefit. HSAs, by contrast, generate a more visible, but narrower, base—those who actively use and value tax-advantaged accounts, often higher-income and more politically engaged. That shift matters because sustainable health reform usually rests on wide, cross-class buy-in. By moving toward HSAs, Republicans may be trading a mass but diffuse constituency for a smaller, more ideologically aligned one. In the long run, that could make federal health support more vulnerable to cuts and cyclical redesign. It raises a deeper question: should health financing be built around a universal logic—everyone in, everyone protected—or segmented tools tailored primarily to those best equipped to navigate complex financial products?
Like this article? Share it with your friends!
If you find this article interesting, feel free to share it with your friends!
Thank you for your support! Sharing is the greatest encouragement for us.